The cornea is the transparent front part of the eye, like the glass on a watch, that helps focus light so we can see well. When the cornea is diseased or damaged it must be treated. If the application of conventional therapy cannot improve vision, there remains an operative method of treatment by corneal replacement, which is called corneal transplantation or keratoplasty.
What is a corneal transplant and what does it achieve?
It is an operation where a diseased cornea through which a person cannot see is replaced by a healthy clear donor cornea of the deceased. Corneal transplantation aims to achieve better vision, reduce pain, and maintain eye stability.
What are the reasons why someone should go for a transplant?
The most common causes are corneal diseases such as Fuchs endothelial dystrophy, Pseudofaccal Bullous Keratopathy, Stromal Corneal Dystrophies, Keratoconus, corneal scars after bacterial, fungal or virus infections and corneal injuries.
Are there different types of transplants and what needs to be done before surgery?
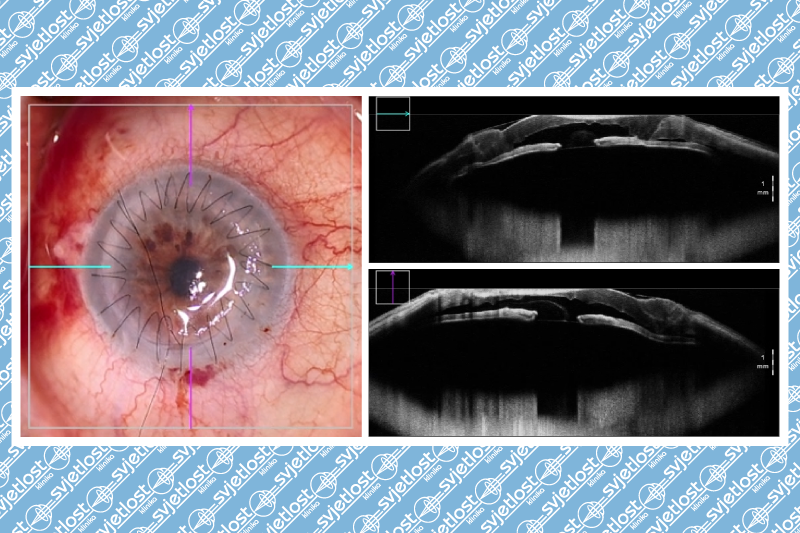
Corneal transplantation can be performed as a full-thickness corneal transplant (perforated keratoplasty) or as transplantation of only the diseased part of the cornea (lamellar corneal transplantation), depending on the patient’s eye condition. Before the procedure, it is necessary to determine the patient's eye condition, assess overall health, and coordinate chronic therapy if the patient is taking it (e.g. anticoagulants should not be taken 3 days before surgery if an internist or general practitioner deems it possible). It is also necessary to do preoperative blood and ECG tests. On the day of the operation, you should come on an empty stomach and bring the reports.
How long is the waiting time for surgery?
The wait depends on the availability of tissue in the eye banks and can be from a few weeks to a few months.
How long does the operation last and what to expect after the procedure?
The procedure itself does not last long, about 30-45 minutes if it is not combined with other procedures on the eye. The patients usually stay in the hospital for one night. After the operation, patients have their eyes covered with gauze for a few days, and when the surface layer of the eye heals, the gauze will be removed in accordance with the doctor's agreement. What is important for patients is that the eye does not hurt after the transplant, but there may be a feeling of discomfort, tingling, and burning. It is recommended to be on sick leave for about 3-6 months after the transplant depending on the type of work the person is doing. Therapy is long-lasting and needs to be taken regularly to ensure the success of the transplant. It is in the form of drops, ointments, and gels and will reduce over time. Check-ups are more frequent in the first period, later they become less frequent, and if everything is in order, there is an interval of 1-2 times a year.
What are the complications of the procedure?
No operation is without complications, so complications after corneal transplantation include the possibility of infection, increased intraocular pressure, cataract formation, retinal ablation, and retinal detachment, which is the most common reason for unsuccessful transplantation.
How successful is the transplant?
Corneal transplantation was performed for the first time a little over 100 years ago as the first successful solid organ transplant and today is the most successful procedure in terms of transplants with over 90% success in low-risk cases such as keratoconus and corneal dystrophy, about 80% in scars without blood vessels and pseudo facial bullous keratopathies, and the success rate decreases to 60% with a greater presence of blood vessels, scars after herpes virus infection, or in repeated transplants.
Corneal transplantation is an extremely successful procedure that requires an excellent surgeon and a cooperative patient, willing to participate in the treatment process, and come for regular check-ups to ensure maximum success of the operation.